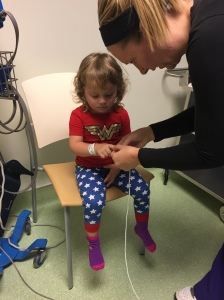
It took several casts before I learned all the ins and outs of what you really should know about your child’s life in a Mehta or EDF cast for early onset scoliosis.
What To Bring To The Hospital on Casting Day:
- Two sets of clothes, loose, stretchy, and comfy and a size or two bigger. Avoid the onesies at the hospital. T-shirts and stretchy pants are ideal.
- Favorite blanket, stuffed animal or toys. We have also found it to be a little helpful to have a brand new toy or something to give to our child once in recovery. Our daughter has an extra tough time coming out of anesthesia and sometimes that balloon or new Elmo doll have helped by being good distractions.
- DVD player or tablet are always helpful and good distractions
- Extra milk, juice, and crackers and other snacks along with their favorite bottle or cup, mainly for the journey home. When you are able to give your child water or juice in recovery, they might prefer it in their own cup or bottle. Mine always has.
- Large waterproof bibs. Vomiting is not uncommon while coming out of anesthesia and you won’t want to deal with vomit and a new cast.
- Gas Drops – most kids have a bit of a tough time coming out of anesthesia. The anesthesia causes gas to build up in their little tummies and can be painful and difficult to get out. The infant gas drops with simethicone help aid in relieving that gas. Be sure to consult with your doctors and nurses in recovery before administering. This tip many have found extremely helpful.
- If your child seems to be having a tough time with vomiting and/or you see that it’s a problem after every cast, be sure to ask your doctors and nurses about the drug Zofran to help with nausea and vomiting.
- Snacks and drinks for you and your significant other. While you probably won’t want to eat, I recommend having at least a little something to eat while your child is in the OR. It can be a very long day emotionally as well as in simple hours. You might not get the opportunity to eat yourself for a long time and you will need your energy.
- Depending on your surgeon and where you live, your child’s casting materials could be simply made of all plaster or plaster with a fiberglass layer on top. In some circumstances if your child has a curve with a low curve degree you might be able to have a waterproof cast for a time period over summer – there are many pros and cons to the waterproof cast and should be discussed with your doctor. Back to the typical casts, they are generally padded on the edges and taped with moleskin and then secured with tape or coban. You can purchase fancy printed duck tapes (get the Duck Tape brand – the Scotch brand is not sticky enough and doesn’t adhere well) and coban to give your child’s cast some fun “flair” . I’ve heard you can even use fabric and modge podge to decorate a cast. That is something you’d want to do at home though.
- If your child has a knit rite shirt on underneath the cast and it can be removed at some point if it’s not cut and taped to the cast. Some surgeons cut it and tape it making it so you can’t remove it. If yours isn’t cut and taped, get an extra shirt from the hospital. Being able to remove that shirt and wash it is highly beneficial for multiple reasons. At least that’s what we have found. It’s not as difficult as it seems either. Here’s a video on how to go about changing that shirt. If your hospital and/or insurance won’t cover extra shirts you can order them here at a very affordable rate (scroll all the way down)
- This is a big one, before you leave be sure you and your nurse and/or casting technician examine the cast to make sure it’s trimmed properly. Check while holding your child and also while your child is sitting. Check to make sure it isn’t too long and hits the hips or legs too much when sitting. Also check the chest bar to make sure it isn’t too high when your child is sitting and it doesn’t hit or come to close to their chin. Make sure it’s not too high under their arms and your child is able to put his or her arms down comfortably.
- ** If you aren’t lucky enough to get an early casting time and are stuck with a mid-day to afternoon casting. Many, including us, have found it’s helpful to let your child stay up late, as late as they can and give them food and drink late as well and then let them sleep in as late as possible. This will help with their desire for food and drink which they can’t have hours and hours before casting. Late night cookies and ice cream – whatever it tales to fill their little bellies really helps.
What To Expect The First Couple Of Days In The First Cast:
I’m not going to sugar coat it, the first cast can be very hard, for everyone. Even after you read all of this and prepare as much as you can, it’s really hard to know what exactly it’s all like.
- Don’t be surprised if your little one is upset, uncomfortable, and hard to console, grumpy or frustrated. And if you’re lucky, your kiddo might just be a little uncomfortable and not show it as much. However your child reacts, it’s normal and TEMPORARY. Kids are super resilient. I’m continually amazed at how resilient they are.
- Their balance might be off not only from the anesthesia but they have also just had their spine twisted and rotated into a straighter shape, it could take a little bit of time for your child to adjust to their new balance. Anesthesia can also cause them to be a little loopy for several hours and that too can throw their balance off.
- Some kids struggle more than others at first to walk, crawl or just plain get around but don’t worry they will. The casts can weigh between 2-4 pounds! That’s a lot of weight on little ones! But don’t be surprised if your little one develops super strong legs by time that first cast comes off.
- In some cases, casted children need to relearn, or invent new ways to maneuver. For example, getting up off the floor can be difficult or bending over to get an object was difficult but like I said these kiddos are pretty resilient and most will find new ways to accomplish tasks at hand. Be patient and help guide them when they are trying new maneuvers. If at any point you are concerned your child is having too much difficulty or not being able to do things they used to, don’t hesitate to contact your surgeon or nurse. That’s what they are there for.
- Sleep can be tough the first few nights. The first night of a new cast we have generally had Nora sleep with us, that’s probably more to put our own minds at ease. We also have a standard sized adult memory foam pillow in her crib which she prefers to sleep on with her head and half of her back on the pillow. Many kids find a bigger pillow more comfortable.
- Don’t be alarmed if your child doesn’t seem to eat as much as they did before the cast in a sitting. Those casts are designed to be nice and snug so it makes sense for a child to feel fuller faster in a cast. We have found smaller more frequent meals help.
- Don’t worry, in a few days your child will be back to doing almost all the things they were before. And you will find a big huge smile on your face when that happens. Here’s what my Nora was like just a few days later http://youtu.be/ueeOTdRFt2o
What To Have On Hand At Home & What To Do To Prepare For Casting Life:
- Moleskin – you will need this if and when any current moleskin becomes loose or wears of the cast. You will also need it if you find an area becoming tight and causing some redness to your child’s skin. Adding extra padding and protection will help. Ask your surgeon or casting technician for extra when you are at the hospital
- Aquaphor – Our surgeon advised us to use this every couple of days on our daughter’s skin under her cast. We squeeze some fingers in there and try and get a good layer on. It helps keep her skin smooth and from drying out or being prone to sores
- If minor skin breakdown occurs, add extra moleskin to the cast in the area where the skin is red or is beginning to blister. Use Mepilex bandages (these are hard to find in drugstores but are available on Amazon) on the sore or blister type band-aids. Be sure to keep the rest of the skin well lubricated with aquaphor to help prevent further skin issues.
- Aviation style tin snips in the strongest gauge possible. And in addition, you should watch a video on how to remove a cast with tin snips. I say this in case of an emergency and you have to get that cast off fast. It’s better to be prepared and know what to do in an emergency than to panic and scramble. Since writing about this here, this now something our surgeon suggests to all his new casting patients. Also, if you choose and/or are given the opportunity to remove your child’s cast yourself you will need these. We have found removing the cast ourselves to be a big help in so many ways. More on that later.
- Speaking of emergencies – talk to your doctor about what you need to know and what you should do in certain emergencies. There are many opinions and advice on CPR and chocking/ Heimlich maneuver approaches to children in casts.
- Many families have found beanbag chairs to be very helpful for the newly casted children to help them with positioning and comfort.
- The smaller convertible infant car seats might not work well once your child is casted. They might be too big for the seat or it could hold them in an uncomfortable position where the cast rubs. The Britaxx Roundabout had been recommended to us from other parents. I’ve also heard some hospitals have various car seat models on hand specifically for infants and toddlers in casts and will loan them out.
- In the event your child shoves something he or she shouldn’t down his or her cast like rocks, food or toys and you can’t reach it with your fingers, the best way to get them out is to first remove the knit rite shirt and see if that does it. If it doesn’t, you will want to thread a pair of panty hose vertically through the cast and “floss” the cast up and down all around. That should pull the little things out. This ‘flossing’ method is also great to use if your child has an itch that just needs to be scratched a little. If it’s dirt or sand you are trying to get out try using a hair dryer on a cool setting.
- If you are planning any travel with your kiddo, even car travel that’s a good distance, be sure to bring your “cast upkeep” goodies with you. Including an extra shirt (if your cast uses a removable shirt) moleskin, duck tape, wipes, a bib, and of course your tin snips. This was a great tip from a mom whose child got car sick and they weren’t close to home. She learned this one the hard way.
Diapering:
- Every child is different and every cast can fit and be a little different which can affect diapering. What works for one child might not work others. Diapering can be a bit of trail and error. Here are the tips many others have experimented with.
- Huggies Overnights –just for nighttime diapering. These suckers hold a lot and one of the last things you want to worry about is a diaper leaking up into the cast and having to clean/dry that. We’ve found this to be the best brand.
- Even regular day time diapers could have a tough time staying up and in place. You might have to try going back down a size to get a good fit. Or you might find you have to fold the top over in the back and in the front to fit under the cast and then secure nice a snug.
- If you find you are having fit issues and/or leakage problems experiment with diapering options. Many moms have remarked that pull-ups stay on better than diapers and I’ve heard a few mom’s swear cloth diapers was their best solution. Some have found using a shoe horn to help push the back of the diaper into the cast in the back to make it secure helps.
- Poise pads or other feminine pads can be added to diapers for even extra leakage protection and are also a good idea to use in the back of a diaper if your child has any stomach or intestinal illnesses, to help avoid the potential diaper blow out up into the cast.
- If your child has a diaper leak or gets his or her cast wet try drying it out as best you can with towels or a shammy and use a hairdryer on a cool setting off and on as much as you can. If you have a knit rite shirt that’s removable, take it off and wash it. If yours doesn’t come off, pull it down below the cast as much as you can and lightly wash with soap and blow dry.
Sponge Baths:
Sponge baths can be a challenge for some especially my child, even after five casts she still despises the sponge bath and so do we.
- We have tried multiple ways to go about the sponge bath. We were lucky in that she didn’t have much hair for the first 4 casts so we didn’t feel compelled to have to wash her hair with every sponge bath. At that time, we would set two towels in front of the TV (and in the winter fireplace). Get two large Tupperware containers of water. One for soapy water the other for rinsing. We would lay her down on the towel and wash all her exposed skin as quickly as we could and rinse and dry simultaneously. Now we lay a towel down on the kitchen counter, lay her on top of it lean her head over the skin and use the hand held nozzle to wash her hair.
- Many mom’s have found success great success with no rinse shampoos, cloths, washes and shampoos, something I think we will try when we get cast number 6.
- There’s even a fellow scoliosis mom who found the Norwex brand of personal care products including their super absorbent microfiber cloth that picks up water, dirt, bacteria, etc. with no need to rinse to be so helpful she now sells for the company! If you are interested contact her at wagoner518@gmail.com.
- The Belly Button- If your child’s cast covers their bellybutton a little it’s not uncommon for moisture to build up in this area and yeast to form. Don’t worry, it’s not harmful although can have a foul odor. If you can, pull the shirt back (if there is one) and clean the belly button every day or two with soap and water. We found q-tips to work great. If it is red and irritated a little aquaphor should help too.
Breastfeeding Tips for Your Casted Child:
- Yes, you can still breastfeed your child. Many mama’s have found the cast to be abrasive on mom’s skin – rubbing it raw. To avoid that breastfeeding moms have suggested the importance of taping the cast. Tape will prevent your skin from rubbing raw.
- Depending on your casting facility, some want you to wait a few days before taping the cast, in the mean time try breastfeeding with a layered nursing shirt or cami so there isn’t skin to cast rubbing.
- Be sure to check with your surgeon about breastfeeding (fluid intake) instructions before each casting. Breast milk is considered clear fluid and has different time restrictions than cow’s milk.
- Many moms recommend having a support person with you the day of casting. someone who is willing to hold and distract your child who might be desperate to nurse and doesn’t understand why mom will not let him or her.
- You will be allowed to breastfeed your child in post-op after your child has been casted.
How to Handle the Summer Heat In A Cast:
- Overheating and heat rash can be very serious in any child let alone one in a body cast where their little bodies have a tough time regulating heat
- Consider investing in a cooling vest (http://www.noeledfcastframe.com/2012-09-27-16-54-53/accessories) – these little numbers are custom made and will most likely last the entire time your child goes through the casting process, best of all they are affordable. These vest hold special ice packs to help keep your child cool. They last for about 2 hours before needing to be refrozen. The vest is safe and easy to use too. They weight less than a pound and a half and should last at least 2 least two years of casting or more. Here’s a picture of one:
-

- It’s important to talk to you daycare provider and/or school because most casted kids can’t handle being out in weather over 80-85 degrees for much more than 20 mins or so at a time. Overheating and heat rash can be serious complications.
- Want your child to experience the fun of running through a sprinkler like other kids? Well you still can. I’ve seen many parents share pictures and stories of using garbage bags and cutting holes in them for legs and feet to protect the cast while allowing them a little fun.
- And of course lots of fluids, breaks and indoor crafts and activities so they are never bored.
At Home Cast Removal:
- Once we learned about at-home cast removal our lives really did change for the better. I wish we had learned about it sooner. Here are some tips on how to go about doing this.
– First, watch a video.
– I think the best time to do it is in the morning when your child’s tummy isn’t full and is the ‘skinniest’.
– Lay your child down on their back by the TV or something to distract them with your hands and scissors any tape and moleskin around the middle of the chest, bar, the belly bar and the tops of the shoulder straps if you have those.
– With the plaster or fiberglass top exposed slide your hand under the top chest bar between your child’s skin and the cast.
– Gently take small ‘snips’ to the cast. Start with the belly bar. It will take some force. Be sure not to push down with the snips to apply pressure and in turn push on your child’s chest or tummy. Do the chest bar next and then a shoulder strap. By then your should be able to pull the cast part and your child should slip out.
– It sounds complicated but it’s really not. Takes less than 5 mins.
Do you have any other tips on how manage day-to-day life in a cast?
Todo lo que necesitas saber acerca de la vida en un yeso y que tu Dr. no te dice
Me tomó varios yesos antes de aprender los ins y outs de lo que realmente debes saber de la vida de los niños en un yeso Mehta o un yeso EDF para escolisis infantil.
¿Què llevar al hospital el día del yeso?
-2 juegos de ropa: suelta, elástica y confortable y una talla o 2 más grande. Evita los camisetas de una pieza. Camisetas y pants elásticos son lo ideal.
-manta, peluche o juguete favorito. También hemos encontrado útil llevar un juguete nuevo o algo que darle una vez que está en recuperación. Nuestra hija tiene un momento duro después de la anestesia y algunas veces un globo o un nuevo Elmo ha ayudado a distraer.
-DVD o una tablet son siempre útiles y buenas distracciones.
-jugo extra, leche y galletas así como otros bocadillos junto con su taza o mamila favorita son útiles para el regreso a casa. Cuando te permiten darle agua o un jugo en recuperación ellos prefieren su taza o botella.
-Baberos largos contra agua : el vomito no es algo extraño al salir de la anestesia y no querrás lidiar con vomito sobre un yeso nuevo.
-gotas para gases: muchos niños tienen dificultad para salir de anestesia. La anestesia causa gas en sus estomaguitos y les puede costar trabajo sacarlos. Las gotas infantiles para el gas con dimeticona ayuda a aliviar las molestias del gas. Asegúrate de consultar con tu doctor y enfermera antes de adminístralas. Este tip resulta muy útil.
Si tu hijo parece tener dificultades vomitando después de cada yeso, puedes pedirle a tu doctor o enfermera que le den Zofran para ayudar con las nauseas y vomito.
-lleva tylenol
-lleva un refrigerio y algo de tomar para tu pareja. Aunque probable te no tengas hambre mientras tu hijo esté en Quirófano debes tratar de comer algo. Puede ser un día muy largo y emocional.
-dependiendo de tu cirujano y donde vivas, el yeso de tu hijo estará hecho ya sea de puro yeso o con fibra de vidrio como cubierta. En algunos casos si la curva de tu hijo es baja podrán ponerle un yeso con material resistente al agua por algún periodo de tiempo -verano-. Sin embargo hay muchos pros y contras que deberás discutir con tu Doctor. Referente a los yesos típicos, estarán normalmente acolchonados en las orillas y cubiertos con “moleskin” y asegurado con cinta. Puedes conseguir duck tape con decoraciones de la marca Duck tape (la de Scotch no pega bien) o usar cinta coban. Incluso he visto casos donde usan tela o usan modgepodge para decorar el yeso. Pero todo esto son cosas que te gustará más hacer en casa.
-si tú hijo tiene una camiseta debajo del yeso y no está pegada o cortada, esta podrá cambiarse en algún momento y puedes pedir otra extra al hospital. Ser capaces de cambiarla y lavarla es muy bueno por muchas razones. Al menos es lo que hemos encontrado. Tampoco es tan difícil cambiarla como parece. Existe un vídeo que te explica cómo cambiarla. Si tu seguro o tu doctor no cubre playeras extras puedes encontrarlas a un precio muy razonable en línea
-esto es muy importante, asegúrate de que la enfermera o el Dr. examiné bien el yeso de tu hijo y que éste se haya sido cortado adecuadamente. Revísalo mientras lo cargas y lo sientas. Checa
Que no esté muy e largo u le roce la cadera o sus piernas mientas está sentado. También checa que la barra del pecho no este muy larga mientras se sienta y que no pegue con su barbilla . Verifica que no este muy alto en las axilas y que pueda colocar sus brazos abajo cómodamente.
Si no tienes suerte de tener programado el yeso muy temprano y lo tienes a medio día o en la tarde. Muchos padres, incluyéndonos, hemos encontrado muy útil dejar que una noche antes tu hijo se duerma lo más tarde posible, darle algo de comer y beber. Ya que esto calmara su deseo de pedir comida o algo de no tomar, lo cual no puede. Hacer antes del yeso. Galletas y helado nocturno puede ayudar.
¿Qué esperar los primeros días con el primer yeso?
No voy a endulzar el proceso, el primer yeso es difícil para todos. Incluso después de leer esto y estar tan preparado como puedas, es muy difícil saber realmente como va ser.
No te sorprendas si tu hijo está alterado, incomodo, difícil de consolar, de mal humor o frustrado. Sí corres con suerte quizás tu hijo solo este un poco molesto y no lo demuestre mucho. Sin embargo, la reacción de tu hijo es normal y TEMPORAL. Los niños son muy resilientes. Yo continuamente me sorprendo.
Pueden tener problemas con el balance a causa de la anestesia pero también debes tomar en cuenta que su columna acaba de ser torcida y rotada a una forma mas derecha, así que tomara algo de tiempo para que tu hijo se ajuste a su nuevo balance. La anestesia puede causar que este un poco adormilado y fuera de balance horas después de aplicarla.
Algunos niños tiene más problemas que otros para caminar, gatear o hacer su vida normal pero no te preocupes esto pasara. El peso del yeso varia entre 2-4 libras. ¡esto es mucho peso extra para nuestros niños! Así que no te sorprendas si tu hijo desarrolla piernas muy Fuertes una vez que le quiten el primer yeso.
En algunos casos los niños debe de re-aprender o inventor algunas nuevas formas de maniobrar. Por ejemplo, levantar cosas del piso o inclinarse por un objeto puede ser difícil al inicio pero estos niños son tan resilientes que la mayoría encontrara la forma de hacerlo. Sé paciente y ayúdalos a guiarlos a encontrar nuevas formas de hacer las cosas. Sí en algún punto estas muy preocupado porque tu hijo esta teniendo muchas dificultades para hacer las cosas que normalmente hacía contacta a tu doctor o enfermera, que para eso están.
Dormir puede ser difícil las primeras noches. La primera noche en un yeso Nuevo, normalmente dejamos que Nora duerma con nosotros y así estamos más tranquilos. Nosotros también tenemos una almohada tamaño estándar para adulto de memoria en su cuna en la cual ella prefiere dormir. Muchos niños encuentran más cómodo dormir en una almohada más grande.
No te alarmes si tú hijo no come tanto como solía hacerlo en antes de traer el yeso. Estos yesos están diseñados para ser suaves y abrazarlos y eso da una sensación de sentirse satisfechos más rápido. Comidas pequeñas más frecuentes ayuda mucho.
No te preocupes demasiado, en algunos días tu hijo estará hacienda las cosas que hacia antes. Y te verás con una gran sonrisa en la boca cuando eso suceda.
¿Qué debes tener en casa y qué hacer para prepararse para vida en con un Yeso?
Moleskin: (protector de pies para zapatos) Vas a necesitar tenerlo por sí se zafa alguno o se ensucia. Puedes usarlo para las áreas donde esta más a apretado causando alguna irritación- Sirve para tener más protección y suavidad del yeso contra la piel. Puedes pedir más a tu cirujano o técnico de yeso cuando estás en el hospital.
Aquaphor: Nuestro cirujano nos recomendó usarla cada 2-3 días en la piel de nuestra hija bajo el yeso. Nosotros metemos los dedos como podemos y tratamos de poner una buena capa. Ayuda a tener la piel suave y evita tener erupciones.
Extra duch tape o coban
Si una erupción menor ocurre, puede poner extra moleskin en el área donde se está irritando. Puedes usar banditas de Mepilex (éstas son difíciles de encontrar en las farmacias pero las puedes conseguir en Amazon) y ponerlo directo en la irritación. Asegúrate de tener el resto de la piel bien lubricada con aquaphor para prevenir problemas de piel.
Baberos resistentes al agua de varios tamaños, los extra largos con mangas son muy buenos para que tu hijo pueda tener un tiempo de jugar con agua.
Pinzas de estilo de aviación de mayor fuerza posible y como complemento debes de ver el video donde te explican como remover un yeso con estas pinzas. Esto es en caso de alguna emergencia donde debas quitarlo. Es mejor estar preparado y saber que hacer en caso de una emergencia que entrar en pánico. Esto es algo que nos sugirió nuestro cirujano. Incluso, si escoges o te permiten remover el yeso de tu hijo necesitaras saber todo esto. Nosotros hemos encontrado muy bueno en muchos sentidos quitarlo nosotros mismos.
Hablando de emergencias, habla con tu doctor acerca de lo que necesitas saber en caso de algunas emergencias. Hay muchas opiniones y consejos acerca de cómo hacer CPR y atragantamiento o maniobra de Heimlich con niños con yeso.
Muchas familias han encontrado muy útiles las sillas tipo beanbag para darles confort a sus hijos.
Las sillas para infantes de carro pequeñas no funcionan para los niños con yeso. Ellos necesitan una silla más grande y cómoda para evitar que el yeso los roce. La silla BritaxxRoundabout ha sido recomendada por muchos padres. Incluso he escuchado que en algunos hospitales les prestan sillas especialmente recomendadas y probadas para niños con yeso.
En el caso que tu hijo se haya introducido algo a su yeso como piedritas, comida, juguetes y no puedes alcanzarlo con tus dedos, la mejor manera de removerlo es primero quitar la camiseta y ver si eso ayuda. Sí eso no ayuda, puedes utilizar unas pantimedias de manera vertical como si estuvieras usando hilo dental por todo el yeso. Eso deberá sacar lo que fuera se hubiera quedado ahí. Este método de asemejar el hilo dental con la pantimedia puede ser muy útil para calmar la comezón. Sí es tierra o arena lo que tiene adentro también puedes usar una secadora de pelo con aire frio.
Pañales
Cada niño es diferente y cada yeso puede ser diferente a otro y esto afectara la manera en que uses el pañal. Lo que me funcione a mí puede que no funcione para otros. El tema del pañal es algo más de “prueba y error” pero aquí hay algunos tips que han experimentado algunas mamas.
HuggiesOvernights-sólo para la hora de dormir. Estos pañales absorben mucho agua y ayudan a no preocuparse por fugas nocturnas.
Incluso los pañales normales del día puede ser un problema que se queden en su lugar. Quizás puedas intentar tener una talla más chica para tener un mejor ajuste. O quizás te podrá ayudar doblar la parte de arriba y meterlo debajo del yeso.
Sí sigues teniendo problemas de fugas experimenta con varios pañales. Muchas mamás han encontrado mejor el uso de pull ups que los pañales regulares, incluso hay algunas que dicen que los pañales de tela funcionan mejor. Algunas usan un calzador de zapato para tener mejor ajuste del pañal debajo del yeso.
Almohadillas para absorber humedad o toallas femeninas pueden agregarse a los pañales para tener una mejor protección e incluso son buena idea para usarlos como una protección extra si tienen diarrea o algún otro problema intestinal
Sí tu hijo tiene alguna fuga en el pañal o se moja el yeso trata de secarlo lo mas posible con una toalla o con la secadora con temperatura fría. Si tienen una playera removible quítala y lávala. Si no se puede quitar jala la playera lo más que puedas, lávala y sécala con la secadora de pelo.
Baños de esponja:
Los baños de esponja pueden ser un reto, especialmente para mi hija que incluso después de 5 yesos odia los baños de esponja y nosotros también. Hemos tratado múltiples maneras de hacerlo. Fuimos afortunados de que no tuvo mucho cabello los 4 primeros yesos así que no teníamos la necesidad de lavarlo cada baño de esponja. En ese momento, nosotros poníamos 2 juegos de toallas frente a la TC (o frente a la chimenea en invierno) poníamos 2 contenedores de agua grandes, uno para agua con jabón y otro para enjuagar. La acostábamos en las toallas y la limpiábamos en las áreas de piel expuesto lo más rápido posible. Ahora ponemos unas toallas en la cocina junto a lava trastes y hacemos que incline la cabeza para lavar su cabello. Muchas mamás han encontrado muy útiles los shampoos en seco y toallas de limpiezas.
Incluso hay una mamá que han encontrado la marca de Norwex muy útil incluyendo la microfibra súper absorbente que recoge agua, mugre, bacterias etc sin necesidad de enjuagar, puedes contactarla a ella en wagoner518@gmail.com.
Sí tu hijo tiene el ombligo cubierto no será raro que desarrolle algún tipo de humedad o levadura. No te preocupes no es dañino y tiene un olor raro, dulce. Sí puedes y tiene camiseta trata de levantarla y limpia su ombligo con agua y jabón una o dos veces al día. Los q-tips sirven de maravilla y sí esta rojo o irritado un poco de aquaphordebe de ayudar,
Tips para amamantar a tu hijo con yeso
Sí, aun puedes amamantar a tu hijo. Muchas mamás han encontrado que el yeso las roza para esto han sugerido ponerle cinta al yeso. Dependiendo del hospital donde le pongan el yeso, algunos te pedirán esperar antes de que le pongas cinta, así que mientras tanto podrás una playera de lactancia. Asegúrate de preguntar a tu cirujano acerca de amamantarlo antes de cada yeso (por el ayuno de fluidos que debe de existir). La leche materna es considerada un fluido claro y tiene restricciones diferentes que la leche de vaca. Asegúrate de ir con alguien el día de yeso que te ayude a distraer a tu hijo cuando esté desesperado por lactar y no entienda porque mamá o lo puede hacer. Te van a permitir amamantarlo una vez que salga del yeso.
Cómo manejar un yeso en el verano
Sobrecalentamiento y erupciones de calor pueden ser muy serios en un niño con yeso. Considera invertir en un chaleco refrescante (http://www.noeledfcastframe.com/2012-09-27-16-54-53/accessories) – el cual podrá ajustarse y ser usando durante todo el proceso del yeso. Duran aproximadamente 2 horas y después necesitan volverse a congelar. El chaleco es seguro y fácil e usar. El peso es menor a 1 libra.
Bandas refrescantes
Es muy importante que hables con el cuidador de tu hijo o a la escuela ya que los niños en yeso no pueden estar en temperaturas superiores a 80-85 F por más de 20 minutos. Sobrecalentamiento y erupciones de calor pueden ser muy graves. Un ventilador de baterías portátil puede ponerse en la carriola y puede ayudar mucho. Si quieres que tu hijo siga disfrutando de las fuentes que salpican agua puedes hacerlo poniendo algún protector como una bolsa de basura con hoyos que lo proteja del agua. Una cama de agua al aire libre puede ser una gran diversión también. Por supuesto no olvides darles muchos líquidos , las actividades dentro de caso pueden ser muy divertidas también.
Quitar un yeso en casa
Una vez que aprendimos como quitar un yeso en casa fue algo muy bueno para nuestras vidas. Desearía haberlo aprendido antes. Aquí algunos tips:
-Ver el video
-Creo que la mejor hora de hacerlo es en la mañana cuando el estomago de tu hijo no esta lleno y esta desinflamado.
-Acuesta a tu hijo de espaldas viendo la TV o algo que lo distraiga con tus manos y tijeras quita todo la cinta y moleskin que tenga.
-ya con el yeso expuesto o la fibra de vidrio desliza tu mano debajo de la barra del pecho para que quede entre la piel y el yeso.
-Suavemente ve cortando el yeso, empieza con la barra que está debajo del ombligo. Se necesitara fuerza. Asegúrate de no presionar mucho sobre el yeso o el estomago. Una vez que cortes ese sigue con el del pecho y luego con los tirantes de los hombros. Para entonces podrás abrir el yeso y quitarlo fácilmente.
-Puede sonar complicado pero realmente no lo es, no tardas más de 5 mins.
Traduccióntextualpor: Paola Ortega Hernández Santarriaga.
 for peer evaluated published studies on the surgical options. Soon into my searches, YouTube videos popped up that were showing the actual surgeries… like in the OR… right there looking down into the exposed spine. Watching surgical procedures has never grossed me out, in fact, I find them usually fascinating. Many years ago, I actually worked as a veterinarian technician where I got to assist in surgeries and I loved it. But there is something very different about 1. Watching orthopedic surgeries. So much hammering, chiseling, sawing. It’s tough and rough, it’s doesn’t seem as delicate as say watching an open heart surgery. And 2. Knowing that the surgery I was watching might actually be performed on my child adds a whole personal and different element to it. Watching these videos was a mistake. I didn’t watch for long but it was a mixed feeling of fascination, being scared, and feeling sick to my stomach. Looking back I would tell myself, do not watch videos of what your child’s spine surgery will be like. This seems so obvious….I know.
for peer evaluated published studies on the surgical options. Soon into my searches, YouTube videos popped up that were showing the actual surgeries… like in the OR… right there looking down into the exposed spine. Watching surgical procedures has never grossed me out, in fact, I find them usually fascinating. Many years ago, I actually worked as a veterinarian technician where I got to assist in surgeries and I loved it. But there is something very different about 1. Watching orthopedic surgeries. So much hammering, chiseling, sawing. It’s tough and rough, it’s doesn’t seem as delicate as say watching an open heart surgery. And 2. Knowing that the surgery I was watching might actually be performed on my child adds a whole personal and different element to it. Watching these videos was a mistake. I didn’t watch for long but it was a mixed feeling of fascination, being scared, and feeling sick to my stomach. Looking back I would tell myself, do not watch videos of what your child’s spine surgery will be like. This seems so obvious….I know.