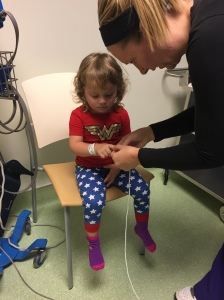
A few weeks ago I got to witness a sweet little two year old girl receive her fourth Mehta/EDF cast. I had the privilege of meeting this baby and her parents last summer when they were just starting the casting process and, like many parents, they were very overwhelmed and scared. We just so happen to have the same amazing surgeon, Dr. Sumeet Garg at Children’s Hospital of Colorado.
If you know me from all the early onset scoliosis support groups, you know I’ve tried to educate myself as much as I can on all things EOS, whether it’s idiopathic, congenital, even some on neuromuscular and syndromic. When it comes to casting, I think I have a great deal of knowledge on not only what it’s like to live day-to-day with a child living in a cast (my child did have nine casts in just about two years), but I also have a good deal of knowledge around the ‘science’ of it and the research behind it. But that’s been all “textbook”.
Over the years there have always been questions that have come up in the support groups where I haven’t fully known what a good answer is. I’ve thought for a long time, if I could just witness an actual casting and ask questions while watching, maybe I would understand better and be able to answer some of these questions better for parents.
Once Nora was finished with casting and we had her surgery behind us, I asked our surgeon if I could come watch one. He said, “I would have let you watch one of Nora’s castings.” That made me chuckle to myself a little bit. I know myself well enough; there was no way I wanted to see that process happen to my own child. I had to wait till we were past it. Taking Nora into the OR for every casting and battling to put her to sleep was just too much. I could never stay and watch the process and actually learn from it. I’d be too worried about her and I’d be an emotional mess. There’s a reason surgeon’s aren’t allowed to operate on their own family members…to me this was kinda like that.
Casting Day:
I had a bunch of paperwork and documentation to provide in order to be given the privilege of observing that day. When I arrived I met Dr. Garg and he took me back to get actual scrubs on and we worked our way to pre-op. He stopped often to chat with other doctors here and there. They were chatting about surgeries from the week before and a special casting as well. He took the time to fill me in a little bit on what each conversation he had was about. It was exciting to hear about new technologies they had implemented in a spine surgery and to hear about a different casting, where they did a waterproof cast.
Pre-Op Meeting:
The whole time we were walking around I was feeling great – excited and calm. A new and strange feeling for me at the hospital. Once we made it to our casting patient’s room and I saw the parents of this little girl my stomach flipped and sank a little. I knew that look on their faces so very well. They didn’t want to be there, they were stressed, tired and more than anything nervous and a little worried. I knew those feelings so well. And yet today, here I was cool as a cucumber; it felt wrong to feel that way. But isn’t that exactly how things are in a hospital setting? Such a stark contrast of feelings and emotions. It’s so hard on families yet can be exciting and rewarding for those who are caring for our children.
After we talked with her parents about the latest x-rays (which she hadn’t had since she started casting; they showed she had some great improvement –so that was exciting to see) the room filled with all the other doctors and nurses who are vital to the whole process. Dr. Garg and I left and made our way back to the OR, this time chatting about everything from our own kids to the holidays and upcoming work trips he had. I love that he shared with me details about his career and what he’s learning and what he’s teaching.

a casting table
Inside the OR:
In the OR, this time from the opposite side door I was used to walking into, I saw the little girl peacefully asleep on the bed. I was hit with a wave of emotions again. I knew this room way to well -all the equipment, the cold temperature in the room, the stark white walls and floor. It was strange being here from the other side without my baby in my arms. I was introduced to everyone in the room and there was brief small talk while they seemed to get everything in place. For the first few minutes, I kept thinking this is what it was like when Nora was in here, this is what went on in here for each one of her castings. That sweet baby on the bed could be Nora. It was just an odd feeling. But I quickly relaxed, because this wasn’t my child and because l looked at her face and saw she was ok, she was peacefully sleeping.
I wasn’t in the room for the intubation, so once we came in she had her IVs, all her monitors in place and the anesthesiologist was monitoring her. It was time to put the knit-rite shirt and stockinette on her body. and getting this special support piece around her neck and face. This is used to support her head and hold her head in the right position once on the casting table.
Now was the hard part. I even asked Dr. Garg at the end what was the hardest part about casting, he said the transfers from the bed to the table and back again. I can totally see why. It’s a lot to move a limp child who is intubated and has a bunch of wires and monitors attached to them over to this strange looking casting table, where their bottom rests or balances on this tiny 2-3 inch bar.
A lot of people are involved in the transfer, holding, and supporting her body and limbs. Once she was over, they quickly get all the wires out of the way or where they need them. Then a nurse is taking this long line of string like gauze and pulling it up over her hips. That string is then pulled and anchored to the back of the table, creating traction and pulling her torso straight. At the same time her head and the support under her chin is being secured to the opposite end of the table. Next her arms are pulled out straight and secured as well. All of that happened fast, but it was very calculated and done with extreme caution to make sure the child is in place properly and secured properly. I could see very easily how difficult that process can be.
The Actual Casting Begins:
Next she was quickly wrapped with the padding that goes under the cast with extra attention placed on her rib hump. Dr. Garg, assessed her and made a couple of tweaks here and there to how her hips were anchored and the position of her body on the table. He was looking at the mirror under the table that allows him her see her back and make adjustments.

this is not the child I saw casted, but this gives you an idea of what they look like on the casting frame
In no time they were ready to start applying the actual plaster. A nurse was unwrapping the casting material and dipping it in the water to get the plaster going and then handing it to Dr. Garg. He just wraps it around her whole body, round and round. The plaster went on super fast. I had no idea how fast that was. The plaster begins to hardens fast, but not so fast you can’t mold it, unlike the fiberglass, which I will talk about in a minute. Dr. Garg would wrap it round and round and then gently push on points of her spine or chest or even hips. Then he would wrap some more, smooth it out and mold again, applying pressure here and there while he went round and round and the cast began to dry.
The pressure he applied, he explained was always with the palm of his hand. If you use fingers when applying pressure you can create pressure points which would not be good. The derotating aspect of the cast application was, what appeared to me, as the hardest part of the cast application. To me it looked not only like a learned skill, but something learned over time that becomes instinctual almost while also being a bit of an art. That’s my best way of describing it. He would gently push from the front and back to shape the cast and would repeat that over and over….smoothing, molding, applying pressure and shaping. He explained, knowing where her curve was from x-rays and her rib hump determined where exactly he would apply the pressure.
I asked how much correction he thought he got. He said he didn’t know for sure but he knew he did get correction. He said surgeons can’t really tell how much without an x-ray. This is something I’ve been wrong on for awhile. I was under the impression surgeons could tell approximately how much correction they were getting while applying the cast and that’s something I’ve said to parents. I’m glad I know better now. It makes more sense to me now why some doctors do in-cast x-rays after every single casting. I personally don’t know if that changes anything or if I’d like that many x-rays but I have a better understanding now why many do.
During this entire time the anesthesiologist was monitoring all her vitals. The cast application process and the pressure involved in the derotation, does put stress on the respiratory system. It is a snug plaster cast being applied to the entire torso. There is no tummy opening yet. This is why intubation is so very important. That intubation protects the airways.
The biggest surprise to me so far was that the process is much gentler than I imagined. I imagined it was a lot of pulling the body in traction to get it in place and then lots of pushing and pressure to actually derotate the spine. It wasn’t like that. Yes, there was some pulling and pushing but it was gentle. I was amazed and relieved!
That being said, I’m still shocked to hear there are some surgeons applying casts on kids while they are awake. There is simply no way, in my mind, that can be done on a child who is awake. One, it would be extremely traumatic for the child, heck it would be tough for even an adult to do that I think, being tied and pulled into place and can’t really move. Two, I have to imagine a young child would be crying hysterically, with their lungs taking in so much air in and out I don’t know how you would get the cast to be fitted properly around the torso. And lastly, how can you assure an awake child is receiving the right traction? How can you get them in place on a proper casting table when they are awake? I simply cannot imagine how it could be done properly and effectively.
Which brings up the next surprise, I still don’t understand how a surgeon makes sure the cast is sung, not tight and not loose. It has to be with how the plaster is smoothed on and how and where pressure is applied. It’s all in the feel I think. To me, that seems like another part that clearly takes practice.
Next up, they applied the fiberglass top layer. This went fast too and this is where I could very easily see the difference in what you can do with plaster and what you can do with fiberglass. Dr. Garg showed me how you can mold and get better hold with plaster. It was very obvious watching to see how well the plaster works for shaping and molding. The fiberglass, it just doesn’t move the same or have the same strength as plaster. It’s more rigid and it hardens faster. I could see how fiberglass just isn’t going to hold the derotation in place like plaster would.
This was a big take away for me. I know there are a handful of surgeons who are only casting using fiberglass. They clearly have had some success but I also think I understand why there are still many who aren’t seeing success; – Could it be related? Obviously, I can’t say for sure but I know if my child had idiopathic scoliosis, with a significant curve, that had the potential to being “cured” I would not want a fiberglass only cast.
After the Cast is Applied:
At this point this little girl was ready to be moved back to the bed. Again the transfer can be tricky. Once they got her over to the bed the clean up began. Plaster is messy, and with as fast as you have to move there is sure to be some drips here and there. Then it was time to trim the cast. The edges, the tummy cut out, the small hole in the back, and under the arms. Dr. Garg, drew with a sharpie where he wanted to cut first, and then went to it with the casting saw.
After living through many casts, I know firsthand the hardest area to deal with is generally under the arms. No matter how you go about it, the cast will rub and press into the arm. The key is not having it too high where it really pinches the skin and can cause sores. Dr. Garg explained how it’s just a tricky area, you can’t cut it too low otherwise you lose some of the casts integrity where it holds the upper chest area. This was something I didn’t know. But If you don’t trim enough it’s going to rub and cause sores. In the casting support group, this is the area we see parents ask about the most. When we see ones that need trimming, I think it’s because most surgeons probably error on the side of caution and keep it a little high and see if the child tolerates it ok. It is hard to tell exactly how a child is going to move about in a cast when they are on a hospital bed under anesthesia.
After all the cuts were made it was time to pull the padding down around the edges, add the mole skin and apply the duck tape. It was that simple and fast. I know many facilities have an entirely different process for how things are done once the cast is on. Many wait till the child is awake, then they are put under a dryer and then taken to a room for trimming and taping – all while awake. I cannot tell you how grateful I am our surgeon gets it all done in the OR. I told everyone in the room the process other facilities have, the collective response from all was surprise and thankfulness for the processes that are in place at Children’s in Denver.
I think those differences have to do with a couple of things, one, the type of plaster the surgeon is using and two, how thick of a cast the surgeon is applying. That’s my only guess as to why some kids need to be put under a dryer and the process takes longer.
Final Thoughts:
All in all I’m very happy I witnessed this. I have a much better understanding now of how it all works and why certain things are done. I’m happy I was able to see just how gentle the process is overall, much different from what I imagined in my head. If there is any one thing I can impart on parents it’s that a properly trained surgeon with experience casting is going to apply the cast in a gentle manner. We often hear parents asking about giving their child Tylenol or ibuprofen after casting because the child might be sore from being pulled and twisted, from what I saw, that’s not the case at all. I think both over the counter medications can have their place post casting, but it’s not for pain from the actual casting itself. I hope parents can take a sigh of relief over that one.
Watching a casting instilled my belief, even more so, that casting was the best option for my child during the time we utilized it. There is nothing barbaric about casting and it can be absolutely life saving for many kids. My wish would be for more pediatric orthopedic surgeons and pediatricians, for that matter, to be able to see what I did and see how casting works. I know that would save more children from years and years of complex surgeries.